Microbiome: The Life-Giving Life
The young man walked up to the door, dropped off a bag full of feces and walked away. No, this wasn’t some adolescent prank designed to cover someone’s front porch with burnt smelly waste; this was a medical donation. The donor was providing healthy gut flora in the form of feces in order to be injected into someone suffering from a gut disease like Crohn’s, Candida, or irritable bowel syndrome.
“It’s disgusting to me as well,” says Dr. Tom Borody who helped pioneer the medical treatment called fecal transplant. But according to the growing data, it works. Fecal transplants have been shown to have a 91 percent cure rate for clostridium difficile and may also help heal IBS, colitis, and autoimmune disease. There are even documented cases where fecal transplants have actually saved a patient’s life.
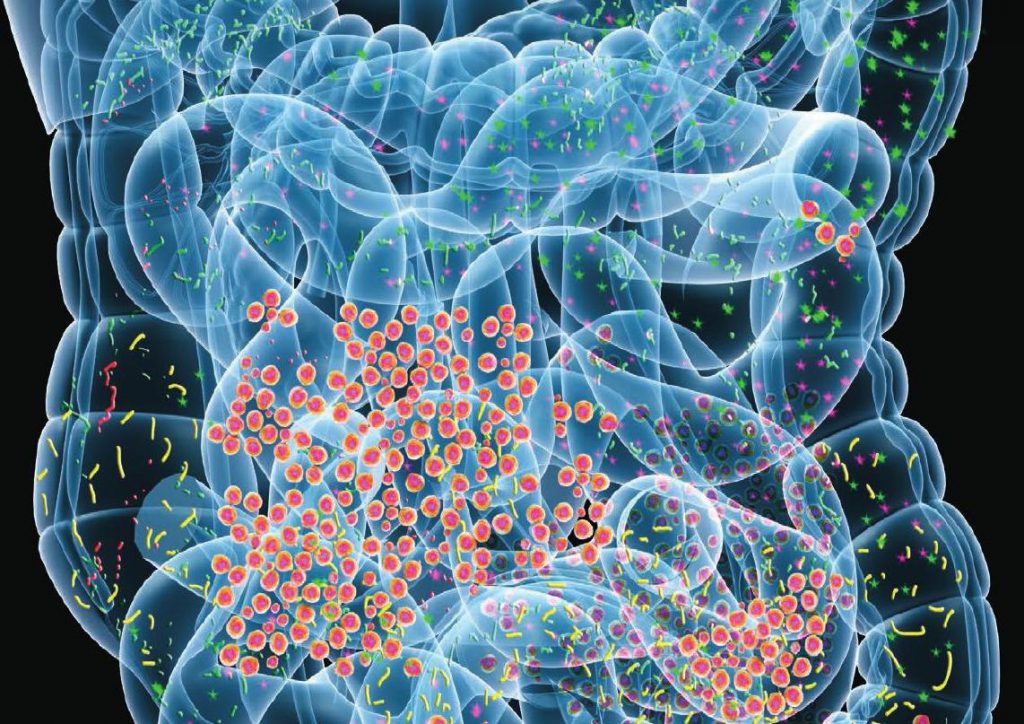
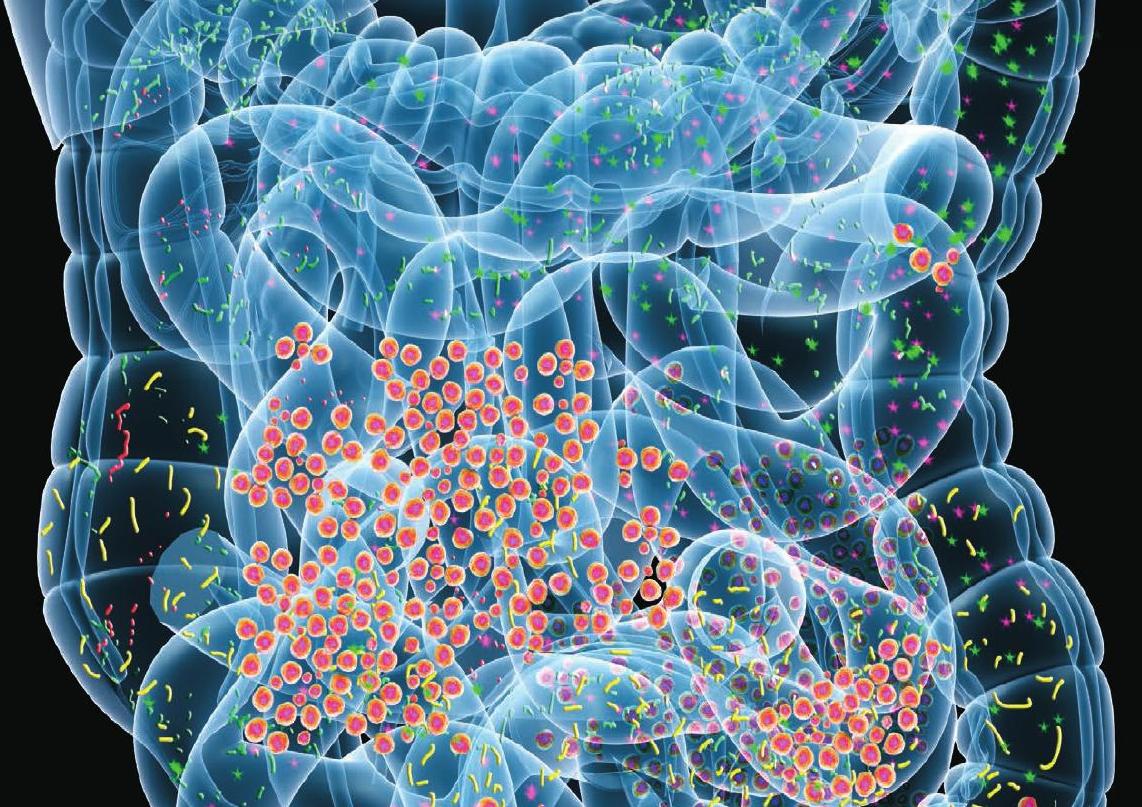
This treatment works on the shocking revelation that what you think of as you is not really just you. On your teeth, on your skin, and in your gastrointestinal tract, trillions of microbiota (from bacteria to archaea to fungi and viruses) live on you in a mutually beneficial symbiosis—they need us to live, but we also need them to live and maintain health. It is widely estimated that there are at least three times as many non-you cells in or on your body as there are your cells. We have over 1000 trillion bacteria inside and on our bodies (which equates to about three to four pounds) that we are dependent on for digestion and gastrointestinal health. Healthy intestinal flora aid the body in everything from digestion, fighting illness, and synthesizing vitamins to psychological wellbeing and weight management.
The problem with many modern medications and other lifestyle choices is that they are harmful or prohibitive to these natural flora. As described in the previous section, someone with a bacterial infection may be prescribed an antibiotic, which will usually kill the pathogen, but also has the unintended consequence of killing hosts of healthy bacteria.
When antibiotics are ingested, the natural balance of those bacteria are thwarted and a whole host of problems can result. Furthermore, when enough good bacteria die, the yeasts in the digestive system take over. Yeast overgrowth can be found to cause a host of health problems including leaky gut and irritable bowel syndromes as well as food allergies. Newer research continues to make new discoveries about the importance of the microbiome, which seems to be particularly vulnerable to the detriment of antibiotics in infants and children. Taking antibiotics may get rid of your bacterial infection, but end up leaving you with IBS.
As Dr. Borody has demonstrated, there are ways to compensate and treat an unhealthy microbiome, but surely the goal should be avoiding damage in the first place. The effects aren’t limited to gastrointestinal flora and gut diseases. One study showed that mice given Mycobacterium vaccae prior to and during a maze learning task demonstrated a reduction in anxiety-related behaviors and maze completion time. In essence, increased healthy bacteria helped in brain ability.
We’re still learning the extent to which our microbiomes affect our health, but one thing is clear: it is substantial. Here is a summary of the latest literature for each microbiome and tips on how to improve them for ultimate wellbeing.
Skin
The skin acts as a barrier to deter the invasion of pathogenic microbes. The human skin contains microbes that reside either in or on the skin and can be residential or transient. Resident microorganism types vary in relation to skin type on the human body. A majority of microbes reside on superficial cells on the skin or prefer to associate with glands. These glands such as oil or sweat glands provide the microbes with water, amino acids, and fatty acids. In addition, resident bacteria associated with oil glands are often Gram-positive and can be pathogenic.
One study of twenty skin sites on each of ten healthy humans found 205 identified genera in nineteen bacterial phyla, with most sequences assigned to four phyla: Actinobacteria (51.8%), Firmicutes (24.4%), Proteobacteria (16.5%), and Bacteroidetes (6.3%). A large number of fungal genera are also present on healthy human skin, with some variability by region of the body; however, during pathological conditions, certain genera tend to dominate in the affected region. For example, Malassezia is dominant in atopic dermatitis and Acremonium is dominant on dandruff-afflicted scalps
Eye
A small number of bacteria and fungi are normally present in the conjunctiva of the eye. Classes of bacteria include Gram-positive cocci (e.g., Staphylococcus and Streptococcus) and Gram-negative rods and cocci (e.g., Haemophilus and Neisseria) are present. Fungal genera include Candida, Aspergillus, and Penicillium. The lachrymal glands continuously secrete, keeping the conjunctiva moist, while intermittent blinking lubricates the conjunctiva and washes away foreign material. Tears contain bactericides such as lysozyme, so that microorganisms have difficulty in surviving the lysozyme and settling on the epithelial surfaces.
Gastrointestinal Tract
Gut flora has the largest numbers of bacteria and the greatest number of species compared to other areas of the body. The relationship between some gut flora and humans is not merely commensal (a non-harmful coexistence), but rather a mutualistic relationship. Some human gut microorganisms benefit the host by fermenting dietary fiber into short-chain fatty acids (SCFAs), such as acetic acid and butyric acid, which are then absorbed by the host human.
Intestinal bacteria also play a role in synthesizing vitamin B and vitamin K as well as metabolizing bile acids, sterols, and xenobiotics. The systemic importance of the SCFAs and other compounds they produce are like hormones and the gut flora itself appears to function like an endocrine organ. The dysregulation of the gut flora has been correlated with a host of inflammatory and autoimmune conditions.
But the gut microbiome doesn’t just affect digestion as the gut-brain connection has also been well-documented. A systematic review of 15 human randomized controlled trials from July 2016 found that certain commercially available strains of oral probiotic bacteria for 1–2 months are effective in treating certain central nervous system disorders, including anxiety, depression, autism spectrum disorder, and obsessive–compulsive disorder, and improved certain aspects of memory.
Gut health promotes overall health for the entire organism and conversely, unhealthy lifestyles also contribute to disrupt healthy gut flora. In an article published by Musso et al., it was found that the gut microbiota of obese individuals had more Firmicutes and less Bacteroidetes than healthy individuals. Furthermore, a study done by Gordon et al., confirmed that it was the composition of the microbiota that causes obesity rather than the other way around. This was done by transplanting the gut microbiota from diet-induced obese (DIO) mice or lean control mice into lean germ-free mice that do not have a microbiome. They found that the mice transplanted with DIO mouse gut microbiota had significantly higher total body fat than the mice transplanted with lean mouse microbiota when fed with the same diet.
What’s more important than the benefits of healthy gut flora is how we get it: during vaginal birth. At the end of pregnancy, the mother’s gut flora travels to her vagina and babies born through the vaginal canal intake non-pathogenic, beneficial gut microbiota, establishing a long-term microbiome. However, the gut microbiota of babies delivered by C-section harbors more pathogenic bacteria such as Escherichia coli and Staphylococcus and it takes longer to develop non-pathogenic, beneficial gut microbiota.
Oral cavity
As disgusting as it may be, our mouths are really our personal Petri dishes—the perfect environment for the growth of characteristic microorganisms. It provides a source of water and nutrients, as well as a moderate temperature. Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.
Bacteria accumulate on both the hard and soft oral tissues in biofilm allowing them to adhere and strive in the oral environment while protected from the environmental factors and antimicrobial agents. Saliva plays a key biofilm homeostatic role allowing recolonization of bacteria for formation and controlling growth by detaching biofilm buildup. It also provides a means of nutrients and temperature regulation. The location of the biofilm determines the type of exposed nutrients it receives.
Oral bacteria have evolved mechanisms to sense their environment and evade or modify the host. However, a highly efficient innate host defense system constantly monitors the bacterial colonization and prevents bacterial invasion of local tissues. A dynamic equilibrium exists between dental plaque bacteria and the innate host defense system.
This dynamic between host oral cavity and oral microbes plays a key role in health and disease as it provides entry into the body. A healthy equilibrium presents a symbiotic relationship where oral microbes limit growth and adherence of pathogens while the host provides an environment for them to flourish. Ecological changes such as change of immune status, shift of resident microbes and nutrient availability shift from a mutual to parasitic relationship resulting in the host being prone to oral and systemic disease. Systemic diseases such as diabetes and cardiovascular diseases has been correlated to poor oral health. Of particular interest is the role of oral microorganisms in the two major dental diseases: dental caries and periodontal disease. Pathogen colonization at the periodontium cause an excessive immune response resulting in a periodontal pocket- a deepened space between the tooth and gums. This acts as a protected blood-rich reservoir with nutrients for anaerobic pathogens. Systemic disease at various sites of the body can result from oral microbes entering the blood bypassing periodontal pockets and oral membranes.
Persistent proper oral hygiene is the primary method for preventing oral and systemic disease. It reduces the density of biofilm and overgrowth of potential pathogenic bacteria resulting in disease. However, proper oral hygiene may not be enough as the oral microbiome, genetics, and changes to immune response play a factor in developing chronic infections.
Have Some Guts
It’s important to note that while the types of microbes present in various regions of the body are consistent across populations, the actual species may differ widely. For instance, a study on the differences between Bangladesh and American kids found that the two groups varied wildly. Also, the Bangladesh children’s gut flora varied from month to month whereas the American kids’ microbiome stayed relatively constant.
The key, though, is diversity. As Human Food Project author Jeff Leach explains, “From the perspective of an ecologist, and more specifically a microbial ecologists, diversity is something you want in an ecosystem.”
That being the case, we recommend consistently experimenting with different foods and techniques that promote healthy gut flora. Here are some ways to improve your GI microbiome:
Eat fermented foods: Fermentation of natural foods reduces sugars and increases probiotics. Foods like yogurt (fermented milk), miso (fermented soy), and kombucha (fermented tea) can taste delicious and diversify your gut flora. Pickling is also a fun activity you can do with vegetables as diverse as cucumbers to watermelon rinds and gives you the same probiotic benefits.
Filter your water: Studies have shown that antiseptics such as chlorine in drinking water can kill off some of the natural gut microbes and negatively affect the immune system. If your source for drinking water is the tap, you should distill and send it through a carbon filtration system.
Eliminate antibiotics: Antibiotics may be helpful in emergencies, but they shouldn’t be a part of your everyday life. Know that when you use them, you are killing extremely beneficial flora as well as the pathogens.
Hand wash dishes: Studies have shown that children who grow up without a dishwasher machine have a lower risk of allergies. Dishwashers are so good at cleaning, evidently, they clean all the good bacteria along with the leftovers. I even avoid soap altogether for my daily oatmeal bowl.
Get a pet: One study showed, predictably, that homes with a dog in them have more diverse microbes throughout and this leads to fewer respiratory issues for children in the household.
Keep old toys: Our second child has a favorite little small stuffed animal that has been everywhere with him, being infused with drool and food particles along the way. It’s gained an endearing nickname, “Stinky Monkey” because it smells pretty bad, but it’s like catnip to our boy. Whenever he’s stressed or distraught, all he needs is a hit of “Stinky” to feel better.
Grow a garden: One of the easiest and most natural ways to improve your microbiome is to grow your own food—in your backyard or in a pot in your kitchen. And when you harvest the insecticide-free food, feel free to eat it without washing. This is akin to the gathering our ancestors survived on for hundreds of thousands of years.
Open your windows: one of my favorite things about spring is the smell of fresh air from newly-opened windows. It also has a health benefit by enabling diverse bacteria to enter the otherwise recycled and filtered air.
For mothers, two more recommendations are vital for the gut health of their children:
Delivery vaginally: Of course, there are extenuating circumstances preventing vaginal delivery, but the natural process of childbirth sets baby up for his or her entire life with a microbiome starter kit.
Breastfeed: Why does human breast milk contains a sugar that babies cannot digest? Because that sugar is there to feed the microbiota that accompanies the milk. These microbes are known to improve the immune system, reduce risk of infection, and aide in cognitive development.