STUDY: COVID Spike Protein Goes Rogue After Infection and Vaccination, Rewires Human Biology
A groundbreaking study published in 2024 on ResearchGate, titled “Effects of SARS-CoV-2 Spike S1 Subunit on the Interplay Between Hepatitis B and Hepatocellular Carcinoma Related Molecular Processes in Human Liver,” sheds new light on the complex interactions between SARS-CoV-2, hepatitis B virus (HBV), and hepatocellular carcinoma (HCC). Authored by G. Colonna, this research explores how the Spike S1 subunit of SARS-CoV-2, a key component of the virus responsible for COVID-19, may influence molecular processes in the human liver, particularly in the context of HBV infection and HCC development.
Background: The Spike S1 Subunit and Its Role
The SARS-CoV-2 virus, which caused the global COVID-19 pandemic, has been extensively studied for its respiratory effects. However, emerging evidence suggests it also impacts other organs, including the liver. The Spike protein of SARS-CoV-2 consists of two subunits: S1, which binds to the human angiotensin-converting enzyme 2 (ACE2) receptor, and S2, which facilitates viral entry into cells. Intriguingly, the S1 subunit has been observed to act independently in the body during and after COVID-19 infection or vaccination, interacting directly with human proteins.
In this study, researchers focused on the liver, where the S1 subunit interacts one-to-one with 12 specific human proteins. These interactions were used as “seeds” to map out functional relationships within the human proteome through enrichment analysis, creating an “interactome” that highlights metabolic activities linked to HBV and HCC.
Methods: Mapping the Interactome
The research team employed a sophisticated approach to investigate these interactions. They identified 12 liver-specific proteins that directly bind to the SARS-CoV-2 S1 subunit. Using these proteins, they extracted functional relationships from the human proteome, focusing on molecular processes cataloged in the Kyoto Encyclopedia of Genes and Genomes (KEGG) database. The resulting interactome revealed several pathways connected to HBV and HCC, with a significant number of genes and proteins involved.
The study also drew on clinical reports of COVID-19 patients with HBV, noting cases where HBV reactivated or progressed to HCC. To understand whether these diseases progress independently or share a common pathway, the researchers analyzed the interactome using multiple approaches, including gene counts, signal strength, and statistical measures like false discovery rate (FDR).
Key Findings: Overlapping Pathways and Clinical Implications
The results were striking. The interactome analysis identified 144 genes linked to both HBV and HCC within a total of 676 genes in the network. Specifically:
- Hepatitis B (HBV): 90 of 158 network genes were associated with HBV (KEGG pathway hsa05161), with a strength of 1.22, a signal of 6.91, and an FDR of 2.37 × 10⁻⁶⁷.
- Hepatocellular Carcinoma (HCC): 54 of 161 network genes were tied to HCC (KEGG pathway hsa05225), with a strength of 0.99, a signal of 3.69, and an FDR of 1.38 × 10⁻³¹.
- Shared Genes: 31 genes were common to both HBV and HCC, representing 57.4% of HCC-related genes and 34.4% of HBV-related genes, suggesting significant overlap.
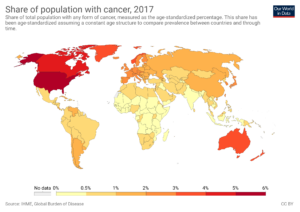
These findings indicate that the S1 subunit of SARS-CoV-2 may influence molecular processes that are critical to both HBV infection and HCC development. The study highlights the heterogeneity of patient responses, noting that the same viral stimulus (S1 protein) can lead to varied outcomes. Some individuals may experience mild or reversible liver damage, while others, particularly those with underlying conditions like metabolic syndrome or mild hepatic inflammation, face a higher risk of progressing to severe conditions like fibrosis or HCC.
Implications: Variability and Personalized Medicine
The research underscores the complexity of liver responses to SARS-CoV-2 in the presence of HBV. The variability in outcomes—driven by differences in immune response, genetic predisposition, and metabolic status—poses a challenge for population-wide predictions. However, it also supports the use of interactomic standards as a reference for understanding these interactions. The study suggests that the S1 subunit may exacerbate existing liver conditions, potentially reactivating HBV or accelerating HCC progression in vulnerable patients.
This variability highlights the need for personalized medicine approaches. By mapping the interactome, researchers can identify key molecular pathways and potential therapeutic targets, paving the way for tailored interventions to mitigate liver damage in COVID-19 patients with HBV or at risk for HCC.
Conclusion: A Call for Further Research
This study provides compelling evidence of the SARS-CoV-2 Spike S1 subunit’s role in influencing liver molecular processes related to HBV and HCC. The overlap between these pathways suggests a potential synergy, where the presence of SARS-CoV-2 could worsen outcomes in patients with chronic HBV or a predisposition to HCC. However, the exact mechanisms—whether these diseases progress independently or through a shared pathway—require further investigation.
As the world continues to grapple with the long-term effects of COVID-19, this research emphasizes the importance of monitoring liver health in patients with pre-existing conditions. Future studies should focus on validating these findings in larger cohorts, exploring therapeutic strategies to block harmful S1 interactions, and refining predictive models to account for individual variability. This work marks a critical step toward understanding the broader impact of SARS-CoV-2 on liver health and its interplay with chronic diseases like HBV and HCC.