Stanford Study Shows How Inflammation Leads to Worse COVID Outcomes
A new study out of Stanford University School of Medicine reveals why some people get severely ill from COVID-19 and others have basically no symptoms.
The key is in the innate immune response to the virus. In a healthy individual, the immune system responds to pathogens in an immediate though somewhat indiscriminate attack on them. It also mobilizes more precisely targeted, but slower-to-get-moving, “sharpshooter” cells belonging to a different branch of the body’s pathogen-defense forces, the adaptive immune system.
In unhealthy patients, however, the “first-responder” immune cells react more sluggishly, perhaps because the patients are dealing with other disease. Researchers found three molecules in severely ill COVID patients associated with lung inflammation in other diseases.
According to the research, the severely ill COVID patients’ immune systems were already bogged down with inflammatory response when infected with SARS-CoV-2, the virus that causes COVID-19. “The underlying causes are unknown, but may be due to an impaired interferon response, and dysregulated inflammatory responses,” the study states.
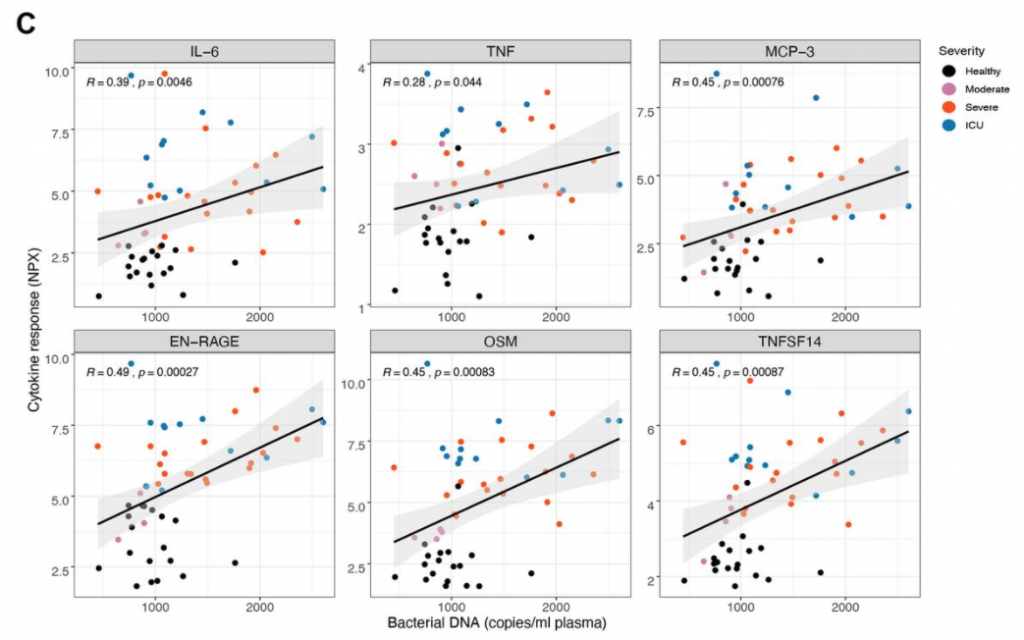
Most patients with severe COVID-19 exhibit enhanced levels of pro-inflammatory cytokines including IL-6 and IL-1β, as well as MCP-1, IP-10 and G-CSF in the plasma…
Strikingly, there were enhanced levels of bacterial DNA and LPS in the plasma, which were positively correlated with the plasma levels of EN-RAGE, TNFSF14, OSM as well as IL-6, suggesting a role for bacterial products, perhaps of lung origin, in augmenting the production of inflammatory cytokines in severe COVID-19.
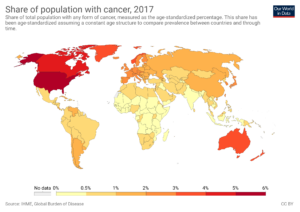
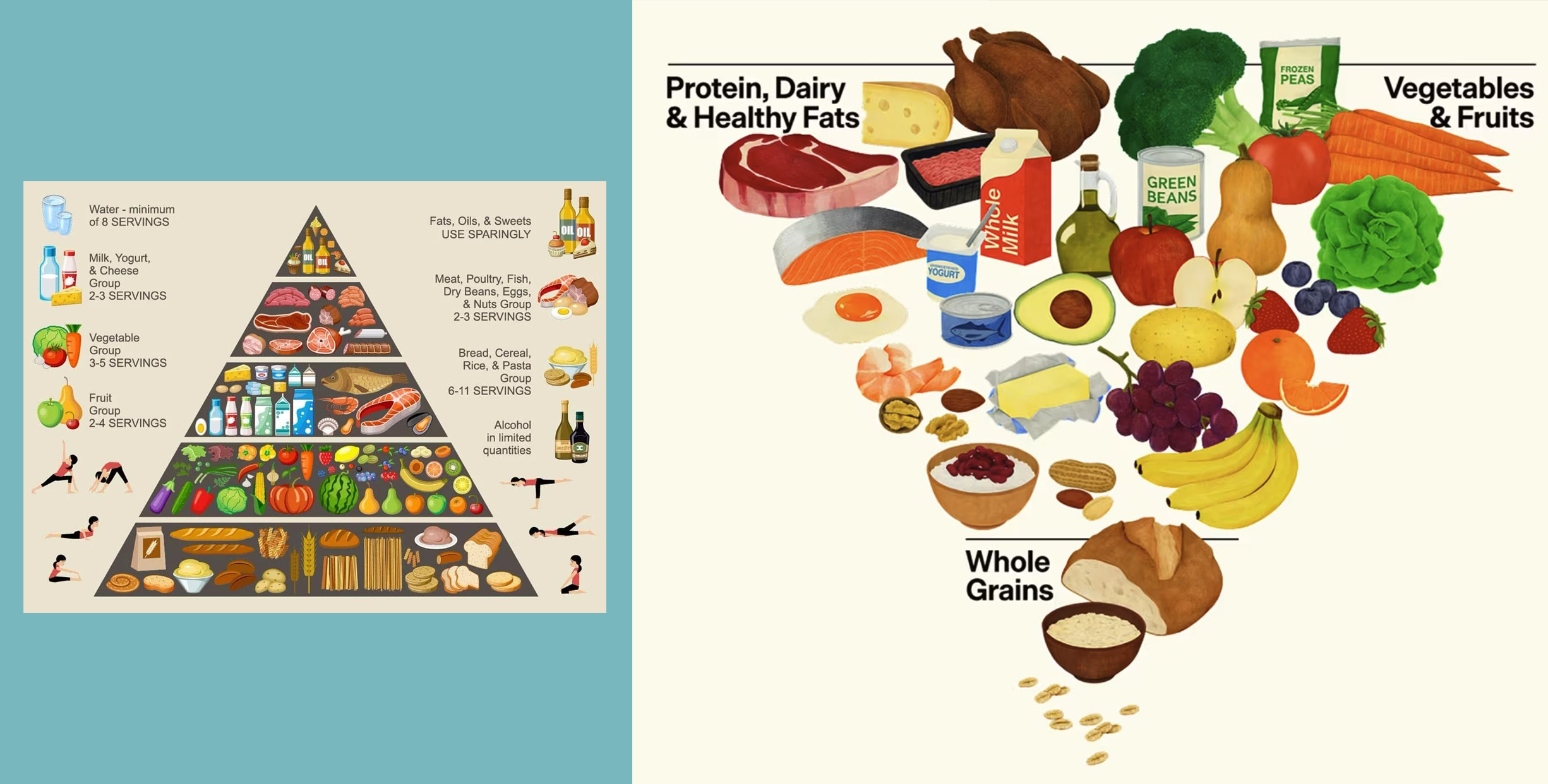
This could explain why people with comorbidities such as cardiovascular disease, diabetes mellitus, chronic lung disease, chronic kidney disease, obesity, hypertension or cancer are at an elevated risk of dying from COVID. It also would explain why an earlier study showed an increased risk of coronavirus severity in people who had received the flu shot, which increases inflammatory response.