You and Your Baby Are What You Eat

Why is maternal diet important? Simply put, because the foods that a mother consumes can assist her baby’s development in utero. This is because the fetus depends on vital micronutrients found circulating in the mother’s blood during pregnancy. Research into recommended maternal diets are expansive, but it is often tricky for moms to navigate the scientific jargon in most studies. Understanding what a good maternal diet is, as well as the long-term effects that diet might have on you and your baby, can be an empowering aspect of your pregnancy.
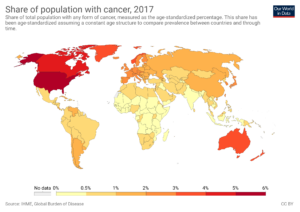
A recent 2015 study published in the Journal of Nutritional Biochemistry suggests that maternal nutrition during the pregnancy and lactation period is likely to affect the development of the child long-term, from fetus, to newborn, all the way through adulthood, as a result of fetal programming and epigenetic regulation (Mennitti 99). Research links the diet of mothers to the development of the kidneys, pancreas, and liver in their babies, with further implications for the child’s risk of future coronary heart disease, stroke, hypertension, and diabetes (Ferreira 1214). Even now, researchers are looking to expand the knowledge of the long-term effects of mothers’ diets on their babies to include potential links to cancer, neurological problems, immunological disorders, autoimmune diseases, allergies, and asthma or asthma related symptoms, as well as behavioral and mental health concerns (Ferreira 1214, O’Neill 2).
Moms need not think of this as scary. Rather, moms should look at all this as good news – it means that mothers should feel empowered to make the right decisions regarding their diets while pregnant because that diet has the ability to benefit their babies’ development in utero, with the long-term effects lasting through her child’s life.
While it is generally known and accepted that what moms eat during pregnancy is likely to affect the development of their babies, it might come as a surprise to learn that a mom’s pregnancy diet often functions as a predictor of their baby’s future diet as well. The World Health Organization (WHO) found that taste programming might occur in utero as a result of an animal study in which junk-food and high-fat diets increased the preference for high-fat, sugary, and salty foods in the offspring (WHO 9). This phenomenon might explain why my first son loved broccoli, which my wife ate nonstop during her second trimester.
Taste is one thing, but epidemiological research suggests that poor nutrition during pregnancy is a contributing factor in global obesity trends. For example, a high-fat diet during pregnancy can actually alter the structure and functionality of the baby’s organs, which, in turn, can influence the child’s susceptibility to certain metabolic disorders (such as type 2 diabetes, cardiovascular disease, obesity, and hypertension) in the future (WHO 7-9, Mennitti 99).
With all that in mind, what can moms do to ensure that their diet is healthy for them and their babies? The first step, perhaps, is understanding the terminology. One important dietary factor is balancing the intake of fatty acids by consuming the right type of fatty acids, like omega-3s. The World Health Organization notes that, since the 1960s, we are consuming less of these essential fatty acids, while the consumption of less ideal fatty acids has increased (WHO 9-10). Animal studies have shown that a high intake of these acids, often called saturated fatty acids or SFAs, have an adverse effect on the offspring’s metabolic regulation (WHO 10).
Omega-3 Fatty Acids
So what do moms need to know about fatty acids? Here’s how the terminology breaks down: the most common fatty acids can be divided into saturated fatty acids (SFAs), trans-fatty acids (TFAs), or polyunsaturated acids (PUFAs). SFAs are most likely to be found in fast and processed foods as well as high-fat dairy products, red meats, and pork (Mennitti 100). TFAs are also present in processed foods (especially snack foods) and baked goods. PUFAs, meanwhile, are those good omega-3 bearing fatty acids that are likely to play a positive role in the development of a baby in utero and in the postnatal stage (Mennitti 99). Of particular importance are the gamma-linolenic acids (GLAs), eicosapentaenoic acids (EPA), and docosahexaenoic acids (DHAs) that are present in omega-3 polyunsaturated fatty acids found in fish as well as some meats. These nutrients (GLAs, EPAs, and DHAs) contribute to healthy circulation and joint mobility and are therefore particularly beneficial as part of a maternal diet plan. DHA, especially, is a fatty acid that helps to regulate the function of the nervous system (as well as brain development) and can be found in a wide range of cold water fish (Judge 531).
Within North America, it is currently estimated that pregnant women consume less than half of their recommended intake of DHA per day (about 200 mg), producing long-term effects on the development of their babies’ nervous systems (Judge 531). Mothers who consume DHA while pregnant (by eating cold water fish and other sources of omega-3 fatty acids) are helping to contribute to their babies’ attention patterns, problem-solving skills, and visual perception (Judge 532). The neurodevelopment of the first 48 hours of a baby’s life, Judge et al. says, is directly related to the mother’s intake of DHA-functional foods during her pregnancy (Judge 532). In more practical terms, what might that mean? Research suggests that that translates into better sleep patterning long-term for the baby (and parents!).
These improved sleep patterns are beneficial to neurocognitive, social, and motor development in infants (Judge 532-534). Not only that – the babies of mothers who consumed DHA while pregnant tend to have fewer sleep “arousals”. Although some degree of sleep arousal in infants is completely normal and actually part of a protective evolutionary response, habitual arousals can lead to sleep fragmentation, which might even lead to infant insomnia (Judge 534).
How can moms ensure that their babies have access to all the benefits of omega-3s and the micronutrients in DHA? Eat fish! And lots of it. Fish is a good source of protein, selenium, zinc, iodine, iron, and other important minerals for the baby’s development in utero. Fish also contains plenty of vitamin B. Oily fish (like salmon) is also a good source of vitamins A and D (FDA). All fish all the time then, right? Well, not exactly. Women of a child-bearing age, especially women who are pregnant or breastfeeding should aim to consume around 2-3 servings of fish per week. That equates to about 8-12 oz. (FDA).
It is also important to ensure that as a mom you are choosing the right fish for you and your baby. Specifically, all those non-mercury storing omega-3 fish. Mercury is absorbed by nearly all fish because of the food that they consume. Some fish, because of their life-span and diet, have greater stores of mercury than others. While a naturally occurring element in water and sediment, over-exposure to mercury can be harmful to the brain and nervous system and that’s why it’s important to understand which types of fish constitute the best choice.
Bearing that in mind, there are loads of good (low-mercury level fish) to choose from, says the FDA. Some popular good fish choices include: anchovies, black sea bass, clams, cod, crab, haddock, lobster, oyster, salmon, scallops, shrimp, squid, tilapia, freshwater trout, and canned, light tuna. However, don’t forget that all fish should be cooked all the way through. Some fish (like salmon) can be served raw, but moms must remember to do what they can to decrease the risk of foodborne illnesses while pregnant by avoiding the consumption of raw fish. A 9-month sabbatical from sushi or sashimi-style raw fish is a good idea.
What are the fish you should avoid while pregnant? The list is actually much shorter and includes: King mackerel, orange roughy, shark, swordfish, tilefish, and bigeye tuna. These fish contain the highest levels of mercury. With all that in mind, it might be tempting to forgo the fishmonger altogether and hit the multivitamin section instead. While taking omega-3 supplements is an option, remember all the other nutrients found in fish that benefit your baby, such as protein, vitamins, and minerals.
Iron
Iron is another element to be mindful of while pregnant. And that can often mean red meat. Although very little iron is needed at the earliest stages of pregnancy (due to the cessation of menstruation), iron transfers to the fetus and placenta significantly increase during the second trimester of pregnancy (and continue to do so!). These iron transfers are vital to the baby’s development of red blood cells (Bothwell 257). The World Health Organization urges mothers to be aware of iron-deficiency anemia, as it can be associated with premature deliveries, low birth-weights, and impaired fetal development (WHO 10).
Getting the right amount of iron can be confusing because iron needs during pregnancy tend to be very personal – determined, in part, by the stores of iron in the body before pregnancy, in addition to the dietary habits of the pregnant woman. Some countries are more at risk for low iron stores. However, those with a varied diet rarely have cause for concern. Iron levels are usually the highest in those who consume large amounts of meat, poultry, and fish. A mother whose diet is high in these sources of absorbable iron before pregnancy is less likely to be affected by iron deficiency during pregnancy (Bothwell 258).
Red meat is one of the best sources of iron, in addition to being a source of protein, vitamin B12, niacin, vitamin B6, iron, zinc, and phosphorous. There are also some of those omega-3 polyunsaturated fats, too (Williams 113). Still, many moms find themselves concerned about red meat. Nutritional studies in Australia and New Zealand show that new food trends tend to favor trimmed external fat in red meat (Williams 113-114). With the exception of minced meat, that means that red meat is leaner than it has been in the past – good news for beef lovers!
But there is more you can do to make sure your baby is getting the right types of nutrients from your diet. Omega-3 fatty acids are more present in beef and lamb than they are in chicken or pork (although fish is still the best source). Even more, pasture-fed beef, although less common in the United States, is a much better source of omega-3s than grain-fed beef (Williams 114).
Other Nutrients
All that beef and fish are great for your high-protein dinner, but what about the rest of the day? A mother’s LoS Hi-Fi snacks should be full of leafy greens – think spinach, kale, and Swiss chard – because they actually help your body to absorb iron. Leafy greens are also good sources of vitamin B and folate, which helps to regulate your metabolism and insulin resistance, in addition to promoting nerve and brain development in your baby (WHO 10). Folate deficiency tends to be associated with anemia, neural-tube defects, congenital heart defects, as well as premature deliveries and low birth-weights (WHO 10). These defects can be combatted through the consumption of folic acid or folic acid-containing multivitamins (Czeizel 4760).
A low intake of folate in conjunction with an excessive intake of vitamin A as well as alcohol can be harmful to the baby’s brain development and growth in utero, especially during the early stages of pregnancy (WHO 11). Because humans do not produce folate, it is important to understand the major sources of it, including fresh (as well as frozen) leafy greens, citrus fruits, wheat, and legumes, like beans, for example (Czeizel 4760). While a diet rich in folate is the first step, it might also be necessary for pregnant women to supplement their folate intake with multivitamins (Czeizel 4760).
With all the changes and excitement of pregnancy, developing a good diet might be the last thing a mom cares about. However, the most important thing to remember is to avoid under- and over-nutrition (WHO 13). Mothers should keep the Zero to Paleo plan through pregnancy but stress LoS Hi-Fi foods high in folate throughout the day and low-mercury fish and beef for dinner. This will give the little one a developmental boost and provide the best chance for a happy and healthy child.
Bibliography
Bothwell, Thomas H. (2000). Iron Requirements in Pregnancy and Strategies to Meet Them. American Journal of Clinical Nutrition, 72(1), 257-264.
Czeizel, Andrew E., Istvan Dudas, Attila Vereczkey, and Ferenc Bánhidy (2013). Folate Deficiency and Folic Acid Supplementation: The Prevention of Neural-Tube Defects and Congenital Heart Defects. Nutrients, 15(11), 4760-4775.
Ferreira, Manuela (2014). Pre-birth world and the development of the immune system: Mum’s diet affects our adult health. Journal of Bio Essays, 36(12), 1213.
Judge, Michelle P., Xiaomei Cong, Ofer Harel, Amber B. Courville, Carol J. Lammi-Keefe (2012). Maternal consumption of a DHA-containing functional food benefits infant sleep patterning: an early neurodevelopmental measure. Early Human Development, 88(7), 531-537.
Mennitti, Laís V., Juliana L. Oliveira, Carina A. Morais, Débora Estadella, Lila M. Oyamab, Claudia M. Oller do Nascimento, Luciana P. Pisani (2015). Type of fatty acids in maternal diets during pregnancy and/or lactation and metabolic consequences of the offspring. Journal of Nutritional Biochemistry, 26, 99-111.
Miller, Rachel L. (2008). Prenatal maternal diet affects asthma risk in offspring. Journal of Clinical Investigation, 118(10), 3265-3268.
Moon, R. J., N. C. Harvey, S. M. Robinson, G. Ntani, J. H. Davies, H. M. Inskip, K. M. Godfrey, E. M. Dennison, P. C. Calder, and C. Cooper (2013). Maternal Plasma Polyunsaturated Fatty Acid Status in Late Pregnancy is Associated with Offspring Body Composition in Childhood. Journal of Clinical Endocrinology Metabolism, 98(1), 299-307.
Netting, Merry J., Philippa F. Middleton, and Maria Makride (2014). Does maternal diet during pregnancy and lactation affect outcomes in offspring? A systematic review of food-based approaches. Nutrition, 11(12), 1225-1241.
O’Neil, Adrienne, Catherine Itsiopoulos, Helen Skouteris, Rachel S Opie, Skye McPhie, Briony Hill, and Felice N. Jackal (2014). Preventing mental health problems in offspring by targeting dietary intake of pregnant women. BMC Medicine, 12(208), 1-7.
U.S. Food & Drug Administration (2017). Eating Fish: What Pregnant Women and Parents Should Know. https://www.fda.gov/Food/FoodborneIllnessContaminants/Metals/ucm393070.htm
Williams, Peter (2007). Nutritional composition of red meat. Nutrition & Dietetics, 64(s4), 113-119.
World Health Organization. Good Maternal Nutrition: the best start in life (2016). (ISBN 978 92 890 5154 5).